Trichotillomania, or hair-pulling disorder, affects many individuals and can have significant emotional and psychological impacts. Cognitive Behavioral Therapy (CBT) has proven to be an effective treatment option for managing trichotillomania, helping individuals understand and change the thoughts and behaviors that contribute to their urge to pull hair. By addressing the underlying triggers and developing coping strategies, people can find relief from this condition.
CBT typically involves identifying the patterns and thoughts leading to hair-pulling episodes. Individuals learn to replace these actions with healthier responses, fostering a greater sense of control and reducing the frequency of hair pulling. This therapeutic approach not only aids in managing symptoms but also promotes long-term recovery.
Trichotillomania Cognitive Behavioral Therapy is a proven approach to managing hair-pulling behaviors. Support and guidance from a qualified therapist can enhance the effectiveness of CBT for trichotillomania. Many find that participating in group therapy or support groups further reinforces positive changes and helps maintain motivation. Engaging in these therapeutic practices can significantly improve one’s quality of life and provide the tools needed to combat this challenging disorder.
Understanding Trichotillomania
Trichotillomania, often characterized by repetitive hair-pulling, can lead to significant distress and impairment. This section outlines its definition, symptoms, prevalence, demographics, and potential causes and risk factors.
Definition and Symptoms
Trichotillomania is classified as a mental health disorder, specifically under the umbrella of obsessive-compulsive and related disorders. Individuals with this condition pull hair from various parts of the body, including the scalp, eyebrows, and eyelashes.
Symptoms may include:
- Visible hair loss: Patches or bald spots may appear due to frequent pulling.
- Tension relief: Many feel tension before pulling and a sense of relief afterward.
- Behavior patterns: Pulling may occur during specific situations, such as stress or anxiety, or even absent-mindedly.
Prevalence and Demographics
Research indicates that trichotillomania affects approximately 1-2% of the population, with varying prevalence among different demographics. It typically begins in adolescence, often around ages 10 to 13, though it can start at any age.
Gender differences are notable; it occurs more frequently in females than males, with a ratio of around 3:1. Cultural factors can also influence prevalence rates, with varying levels of acceptance affecting help-seeking behaviors.
Causes and Risk Factors
The exact causes of trichotillomania remain uncertain, although several factors contribute to its onset. Genetics may play a role, as individuals with a family history of similar disorders may be more susceptible.
Environmental factors, such as significant stressors or traumatic experiences, can also trigger the onset of symptoms. Additionally, certain personality traits, like perfectionism or anxiety, might increase the likelihood of developing this condition. A comprehensive understanding of these factors is crucial for effective treatment strategies.
Cognitive Behavioral Therapy for Trichotillomania
Cognitive Behavioral Therapy (CBT) is a structured, goal-oriented approach that addresses the thought patterns and behaviors linked to trichotillomania. It focuses on helping individuals understand the triggers for hair-pulling and develop coping strategies.
Principles of CBT
CBT is founded on the idea that thoughts, feelings, and behaviors are interconnected. In the context of trichotillomania, individuals learn to identify distorted or negative thoughts related to their behavior.
The therapy aims to change these thought patterns, promoting healthier emotional responses and behaviors. By challenging irrational beliefs, clients can foster self-awareness and reduce the urge to pull hair.
Key principles include cognitive restructuring, exposure therapy, and behavioral activation. Each principle plays a crucial role in helping individuals understand and eventually modify their habits.
CBT Techniques and Interventions
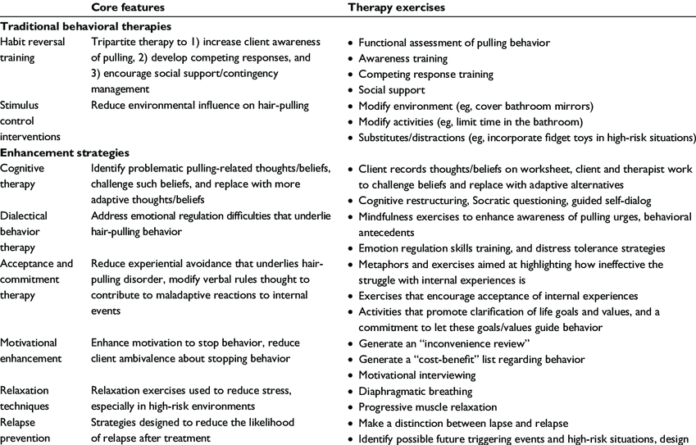
Several specific techniques are used in CBT for trichotillomania. Habit Reversal Training (HRT) is one of the most effective methods. This involves teaching individuals to recognize hair-pulling triggers and substitute the behavior with a compatible alternative.
Another technique is mindfulness, which helps clients stay present and reduce anxiety that may lead to hair-pulling. Utilizing self-monitoring strategies, individuals track their behavior to increase awareness of patterns and triggers.
Group therapy sessions may also provide support and encourage accountability through shared experiences. Psychoeducation is integral, educating clients on the nature of compulsions and offering tools to manage them effectively.
Treatment Efficacy and Outcomes
Research indicates that CBT can significantly reduce the frequency of hair-pulling episodes. Many studies show that patients experience a marked decrease in symptoms over time with consistent therapeutic engagement.
Long-term outcomes suggest that CBT not only aids in symptom management but also enhances emotional regulation skills. Approximately 50% of individuals in structured CBT programs report significant improvements.
Success often depends on factors such as the individual’s commitment and the duration of treatment. Regular follow-ups and booster sessions can further strengthen the gains made during therapy. Evidence supports CBT as an efficacious treatment for trichotillomania, leading to favorable outcomes for many individuals.